Hormone Therapy for Breast Cancer
What are hormones?
Hormones are substances that function as chemical messengers in the body. They affect the actions of cells and tissues at various locations in the body, often reaching their targets through the bloodstream.
The hormones estrogen and progesterone are produced by the ovaries in premenopausal women and by some other tissues, including fat and skin, in both premenopausal and postmenopausal women and men. Estrogen promotes the development and maintenance of female sex characteristics and the growth of long bones. Progesterone plays a role in the menstrual cycle and pregnancy.
Estrogen and progesterone also promote the growth of some breast cancers, which are called hormone-sensitive (or hormone-dependent) breast cancers. Hormone-sensitive breast cancercells contain proteins called hormone receptors that become activated when hormones bind to them. The activated receptors cause changes in the expression of specific genes, which can stimulate cell growth.
What is hormone therapy?
Hormone therapy (also called hormonal therapy, hormone treatment, or endocrine therapy) slows or stops the growth of hormone-sensitive tumors by blocking the body's ability to produce hormones or by interfering with effects of hormones on breast cancer cells. Tumors that are hormone insensitive do not have hormone receptors and do not respond to hormone therapy.
To determine whether breast cancer cells contain hormone receptors, doctors test samples of tumor tissue that have been removed by surgery. If the tumor cells contain estrogen receptors, the cancer is called estrogen receptor positive (ER positive), estrogen sensitive, or estrogen responsive. Similarly, if the tumor cells contain progesterone receptors, the cancer is called progesterone receptor positive (PR or PgR positive). Approximately 80% of breast cancers are ER positive.1 Most ER-positive breast cancers are also PR positive. Breast tumors that contain estrogen and/or progesterone receptors are sometimes called hormone receptorpositive (HR positive).
Breast cancers that lack estrogen receptors are called estrogen receptor negative (ER negative). These tumors are estrogen insensitive, meaning that they do not use estrogen to grow. Breast tumors that lack progesterone receptors are called progesterone receptor negative (PR or PgR negative). Breast tumors that lack both estrogen and progesterone receptors are sometimes called hormone receptor negative (HR negative).
Hormone therapy for breast cancer should not be confused with menopausal hormone therapy (MHT)—treatment with estrogen alone or in combination with progesterone to help relieve symptoms of menopause. These two types of therapy produce opposite effects: hormone therapy for breast cancer blocks the growth of HR-positive breast cancer, whereas MHT can stimulate the growth of HR-positive breast cancer. For this reason, when a woman taking MHT is diagnosed with HR-positive breast cancer she is usually asked to stop that therapy.
What types of hormone therapy are used for breast cancer?
Several strategies are used to treat hormone-sensitive breast cancer:
Blocking ovarian function: Because the ovaries are the main source of estrogen in premenopausal women, estrogen levels in these women can be reduced by eliminating or suppressing ovarian function. Blocking ovarian function is called ovarian ablation.
Ovarian ablation can be done surgically in an operation to remove the ovaries (called oophorectomy) or by treatment with radiation. This type of ovarian ablation is usually permanent.
Alternatively, ovarian function can be suppressed temporarily by treatment with drugs called gonadotropin-releasing hormone (GnRH) agonists, which are also known as luteinizing hormone-releasing hormone (LH-RH) agonists. These medicines interfere with signals from the pituitary gland that stimulate the ovaries to produce estrogen.
Examples of ovarian suppression drugs that have been approved by the U.S. Food and Drug Administration (FDA) are goserelin (Zoladex®) and leuprolide (Lupron®).
Blocking estrogen production: Drugs called aromatase inhibitors are used to block the activity of an enzyme called aromatase, which the body uses to make estrogen in the ovaries and in other tissues. Aromatase inhibitors are used primarily in postmenopausal women because the ovaries in premenopausal women produce too much aromatase for the inhibitors to block effectively. However, these drugs can be used in premenopausal women if they are given together with a drug that suppresses ovarian function.
Examples of aromatase inhibitors approved by the FDA are anastrozole (Arimidex®) and letrozole (Femara®), both of which temporarily inactivate aromatase, and exemestane (Aromasin®), which permanently inactivates aromatase.
Blocking estrogen's effects: Several types of drugs interfere with estrogen's ability to stimulate the growth of breast cancer cells:
• Selective estrogen receptor modulators (SERMs) bind to estrogen receptors, preventing estrogen from binding. Examples of SERMs approved by the FDA for treatment of breast cancer are tamoxifen(Nolvadex®) and toremifene (Fareston®). Tamoxifen has been used for more than 30 years to treat HR+hormone receptor–positive breast cancer.
Because SERMs bind to estrogen receptors, they can potentially not only block estrogen activity (i.e., serve as estrogen antagonists) but also mimic estrogen effects (i.e., serve as estrogen agonists). SERMs can behave as estrogen antagonists in some tissues and as estrogen agonists in other tissues. For example, tamoxifen blocks the effects of estrogen in breast tissue but acts like estrogen in the uterus and bone.
• Other antiestrogen drugs, such as fulvestrant (Faslodex), work in a somewhat different way to block estrogen's effects. Like SERMs, fulvestrant binds to the estrogen receptor and functions as an estrogen antagonist. However, unlike SERMs, fulvestrant has no estrogen agonist effects. It is a pure antiestrogen. In addition, when fulvestrant binds to the estrogen receptor, the receptor is targeted for destruction.
How is hormone therapy used to treat breast cancer?
There are three main ways that hormone therapy is used to treat hormone-sensitive breast cancer:
Adjuvant therapy for early-stage breast cancer: Research has shown that women who receive at least 5 years of adjuvant therapy with tamoxifen after having surgery for early-stage ER-positive breast cancer have reduced risks of breast cancer recurrence, including a new breast cancer in the other breast, and death at 15 years.2
Tamoxifen is approved by the FDA for adjuvant hormone treatment of premenopausal and postmenopausal women (and men) with ER-positive early-stage breast cancer, and the aromatase inhibitor anastrozole andletrozole are approved for this use in postmenopausal women.
A third aromatase inhibitor, exemestane, is approved for adjuvant treatment of early-stage breast cancer in postmenopausal women who have received tamoxifen previously.
Until recently, most women who received adjuvant hormone therapy to reduce the chance of a breast cancer recurrence took tamoxifen every day for 5 years. However, with the introduction of newer hormone therapies, some of which have been compared with tamoxifen in clinical trials, additional approaches to hormone therapy have become common.3–5 For example, some women may take an aromatase inhibitor every day for 5 years, instead of tamoxifen. Other women may receive additional treatment with an aromatase inhibitor after 5 years of tamoxifen. Finally, some women may switch to an aromatase inhibitor after 2 or 3 years of tamoxifen, for a total of 5 or more years of hormone therapy. Research has shown that for postmenopausal women who have been treated for early-stage breast cancer, adjuvant therapy with an aromatase inhibitor reduces the risk of recurrence and improves overall survival, compared with adjuvant tamoxifen.6
Decisions about the type and duration of adjuvant hormone therapy must be made on an individual basis. This complicated decision-making process is best carried out by talking with an oncologist, a doctor who specializes in cancer treatment.
Treatment of advanced or metastatic breast cancer: Several types of hormone therapy are approved to treat metastatic or recurrent hormone-sensitive breast cancer. Hormone therapy is also a treatment option for ER-positive breast cancer that has come back in the breast, chest wall, or nearby lymph nodes after treatment (also called a locoregional recurrence).
Two SERMs are approved to treat metastatic breast cancer, tamoxifen and toremifene. The antiestrogenfulvestrant is approved for postmenopausal women with metastatic ER-positive breast cancer that has spread after treatment with other antiestrogens.7 It may also be used in premenopausal women who have hadovarian ablation.
The aromatase inhibitors anastrozole and letrozole are approved to be given to postmenopausal women as initial therapy for metastatic or locally advanced hormone-sensitive breast cancer.8,9These two drugs, as well as the aromatase inhibitor exemestane, are used to treat postmenopausal women with advanced breast cancer whose disease has worsened after treatment with tamoxifen.10
Some women with advanced breast cancer are treated with a combination of hormone therapy and a targeted therapy. For example, the targeted therapy drug lapatinib (Tykerb®) is approved to be used in combination with letrozole to treat hormone receptor–positive, HER2-positive metastatic breast cancer in postmenopausal women for whom hormone therapy is indicated.
Another targeted therapy, palbociclib (Ibrance®), has been granted accelerated approval for use in combination with letrozole as initial therapy for the treatment of hormone receptor–positive, HER2-negativeadvanced breast cancer in postmenopausal women. Palbociclib inhibits two cyclin-dependent kinases (CDK4 and CDK6) that appear to promote the growth of hormone receptor–positive breast cancer cells.
Palbociclib is also approved to be used in combination with fulvestrant for the treatment of women with hormone receptor–positive, HER2-negative advanced or metastatic breast cancer whose cancer has gotten worse after treatment with another hormone therapy.
Neoadjuvant treatment of breast cancer: The use of hormone therapy to treat breast cancer before surgery (neoadjuvant therapy) has been studied in clinical trials.11 The goal of neoadjuvant therapy is to reduce the size of a breast tumor to allow breast-conserving surgery. Data from randomized controlled trials have shown that neoadjuvant hormone therapy—in particular, with aromatase inhibitors—can be effective in reducing the size of breast tumors in postmenopausal women. The results in premenopausal women are less clear because only a few small trials involving relatively few premenopausal women have been conducted thus far.
No hormone therapy has yet been approved by the FDA for the neoadjuvant treatment of breast cancer.
Can hormone therapy be used to prevent breast cancer?
Yes. Most breast cancers are ER positive, and clinical trials have tested whether hormone therapy can be used to prevent breast cancer in women who are at increased risk of developing the disease.
A large NCI-sponsored randomized clinical trial called the Breast Cancer Prevention Trial found that tamoxifen, taken for 5 years, reduced the risk of developing invasive breast cancer by about 50% in postmenopausal women who were at increased risk.12 Long-term follow-up of another randomized trial, the International Breast Cancer Intervention Study I, found that 5 years of tamoxifen treatment reduces the incidence of breast cancer for at least 20 years.13 A subsequent large randomized trial, the Study of Tamoxifen and Raloxifene, which was also sponsored by NCI, found that 5 years of raloxifene (a SERM) reduces breast cancer risk in such women by about 38%.14
As a result of these trials, both tamoxifen and raloxifene have been approved by the FDA to reduce the risk of developing breast cancer in women at high risk of the disease. Tamoxifen is approved for this use regardless of menopausal status. Raloxifene is approved for use only in postmenopausal women.
Two aromatase inhibitors—exemestane and anastrazole—have also been found to reduce the risk of breast cancer in postmenopausal women at increased risk of the disease. After 3 years of follow-up in a randomized trial, women who took exemestane were 65% less likely than those who took a placebo to develop breast cancer.15 After 7 years of follow-up in another randomized trial, women who took anastrozole were 50% less likely than those who took placebo to develop breast cancer.16 Both exemestane and anastrozole are approved by the FDA for treatment of women with ER-positive breast cancer. Although both are also used for breast cancer prevention, neither is approved for that indication specifically.
What are the side effects of hormone therapy?
The side effects of hormone therapy depend largely on the specific drug or the type of treatment.5 The benefits and harms of taking hormone therapy should be carefully weighed for each woman. A common switching strategy used for adjuvant therapy, in which patients take tamoxifen for 2 or 3 years, followed by an aromatase inhibitor for 2 or 3 years, may yield the best balance of benefits and harms of these two types of hormone therapy.17
Hot flashes, night sweats, and vaginal dryness are common side effects of hormone therapy. Hormone therapy also disrupts the menstrual cycle in premenopausal women.
Less common but serious side effects of hormone therapy drugs are listed below.
Tamoxifen
- Risk of blood clots, especially in the lungs and legs12
- Stroke17
- Cataracts18
- Endometrial and uterine cancers17,19
- Bone loss in premenopausal women
- Mood swings, depression, and loss of libido
- In men: headaches, nausea, vomiting, skin rash, impotence, and decreased sexual interest
Raloxifene
- Risk of blood clots, especially in the lungs and legs12
- Stroke in certain subgroups17
Ovarian suppression
- Bone loss
- Mood swings, depression, and loss of libido
Aromatase inhibitors
- Risk of heart attack, angina, heart failure, and hypercholesterolemia20
- Bone loss
- Joint pain21–24
- Mood swings and depression
Fulvestrant
- Gastrointestinal symptoms25
- Loss of strength24
- Pain
Can other drugs interfere with hormone therapy?
Certain drugs, including several commonly prescribed antidepressants (those in the category called selective serotonin reuptake inhibitors, or SSRIs), inhibit an enzyme called CYP2D6. This enzyme plays a critical role in the use of tamoxifen by the body because it metabolizes, or breaks down, tamoxifen into molecules, or metabolites, that are much more active than tamoxifen itself.
The possibility that SSRIs might, by inhibiting CYP2D6, slow the metabolism of tamoxifen and reduce its effectiveness is a concern given that as many as one-fourth of breast cancer patients experience clinical depression and may be treated with SSRIs. In addition, SSRIs are sometimes used to treat hot flashes caused by hormone therapy.
Many experts suggest that patients who are taking antidepressants along with tamoxifen should discuss treatment options with their doctors. For example, doctors may recommend switching from an SSRI that is a potent inhibitor of CYP2D6, such as paroxetine hydrochloride (Paxil®), to one that is a weaker inhibitor, such assertraline (Zoloft®), or that has no inhibitory activity, such as venlafaxine (Effexor®) or citalopram (Celexa®). Or they may suggest that their postmenopausal patients take an aromatase inhibitor instead of tamoxifen.
Other medications that inhibit CYP2D6 include the following:
- Quinidine, which is used to treat abnormal heart rhythms
- Diphenhydramine, which is an antihistamine
- Cimetidine, which is used to reduce stomach acid
People who are prescribed tamoxifen should discuss the use of all other medications with their doctors.
Selected References
1. Kohler BA, Sherman RL, Howlader N, et al. Annual Report to the Nation on the Status of Cancer, 1975-2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. Journal of the National Cancer Institute 2015; 107(6):djv048. doi: 10.1093/jnci/djv048
2. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet 2011; 378(9793)771–784. [PubMed Abstract]
3. Untch M, Thomssen C. Clinical practice decisions in endocrine therapy. Cancer Investigation2010; 28 Suppl 1:4–13. [PubMed Abstract]
4. Regan MM, Neven P, Giobbie-Hurder A, et al. Assessment of letrozole and tamoxifen alone and in sequence for postmenopausal women with steroid hormone receptor-positive breast cancer: the BIG 1–98 randomised clinical trial at 8.1 years median follow-up. Lancet Oncology2011; 12(12):1101–1108. [PubMed Abstract]
5. Burstein HJ, Griggs JJ. Adjuvant hormonal therapy for early-stage breast cancer. Surgical Oncology Clinics of North America 2010; 19(3):639–647. [PubMed Abstract]
6. Early Breast Cancer Trialists' Collaborative Group (EBCTCG), Dowsett M, Forbes JF, et al. Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet 2015; 386(10001):1341-1352. [PubMed Abstract]
7. Howell A, Pippen J, Elledge RM, et al. Fulvestrant versus anastrozole for the treatment of advanced breast carcinoma: a prospectively planned combined survival analysis of two multicenter trials. Cancer 2005; 104(2):236–239. [PubMed Abstract]
8. Cuzick J, Sestak I, Baum M, et al. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncology 2010; 11(12):1135–1141. [PubMed Abstract]
9. Mouridsen H, Gershanovich M, Sun Y, et al. Phase III study of letrozole versus tamoxifen as first-line therapy of advanced breast cancer in postmenopausal women: analysis of survival and update of efficacy from the International Letrozole Breast Cancer Group. Journal of Clinical Oncology 2003; 21(11):2101–2109. [PubMed Abstract]
10. Mauri D, Pavlidis N, Polyzos NP, Ioannidis JP. Survival with aromatase inhibitors and inactivators versus standard hormonal therapy in advanced breast cancer: meta-analysis. Journal of the National Cancer Institute 2006; 98(18):1285–1291. [PubMed Abstract]
11. Chia YH, Ellis MJ, Ma CX. Neoadjuvant endocrine therapy in primary breast cancer: indications and use as a research tool. British Journal of Cancer 2010; 103(6):759–764. [PubMed Abstract]
12. Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P–2 trial. JAMA 2006; 295(23):2727–2741. [PubMed Abstract]
13. Cuzick J, Sestak I, Cawthorn S, et al. Tamoxifen for prevention of breast cancer: extended long-term follow-up of the IBIS-I breast cancer prevention trial. Lancet Oncology 2015; 16(1):67-75. [PubMed Abstract]
14. Vogel VG, Costantino JP, Wickerham DL, et al. Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 Trial: Preventing breast cancer. Cancer Prevention Research 2010; 3(6):696-706. [PubMed Abstract]
15. Goss PE, Ingle JN, Alés-Martinez JE, et al. Exemestane for breast-cancer prevention in postmenopausal women. New England Journal of Medicine 2011; 364(25):2381–2391. [PubMed Abstract]
16. Cuzick J, Sestak I, Forbes JF, et al. Anastrozole for prevention of breast cancer in high-risk postmenopausal women (IBIS-II): an international, double-blind, randomised placebo-controlled trial. Lancet 2014; 383(9922):1041-1048. [PubMed Abstract]
17. Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P–1 Study. Journal of the National Cancer Institute 1998; 90(18):1371–1388. [PubMed Abstract]
18. Gorin MB, Day R, Costantino JP, et al. Long-term tamoxifen citrate use and potential ocular toxicity.American Journal of Ophthalmology 1998; 125(4):493–501. [PubMed Abstract]
19. Tamoxifen for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists' Collaborative Group. Lancet 1998; 351(9114):1451–1467. [PubMed Abstract]
20. Amir E, Seruga B, Niraula S, Carlsson L, Ocaña A. Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: a systematic review and meta-analysis. Journal of the National Cancer Institute 2011; 103(17):1299–1309. [PubMed Abstract]
21. Coates AS, Keshaviah A, Thürlimann B, et al. Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1–98. Journal of Clinical Oncology 2007; 25(5):486–492. [PubMed Abstract]
22. Arimidex, Tamoxifen, Alone or in Combination (ATAC) Trialists' Group. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the ATAC trial. Lancet Oncology 2008; 9(1):45–53. [PubMed Abstract]
23. Coombes RC, Kilburn LS, Snowdon CF, et al. Survival and safety of exemestane versus tamoxifen after 2–3 years' tamoxifen treatment (Intergroup Exemestane Study): a randomised controlled trial. Lancet 2007; 369(9561):559–570. Erratum in: Lancet 2007; 369(9565):906. [PubMed Abstract]
24. Boccardo F, Rubagotti A, Guglielmini P, et al. Switching to anastrozole versus continued tamoxifen treatment of early breast cancer. Updated results of the Italian Tamoxifen Anastrozole (ITA) Trial. Annals of Oncology 2006; 17(Suppl 7):vii10–vii14. [PubMed Abstract]
25. Osborne CK, Pippen J, Jones SE, et al. Double-blind, randomized trial comparing the efficacy and tolerability of fulvestrant versus anastrozole in postmenopausal women with advanced breast cancer progressing on prior endocrine therapy: results of a North American trial. Journal of Clinical Oncology 2002; 20(16):3386–3395. [PubMed Abstract]
Source: National Cancer Institute.
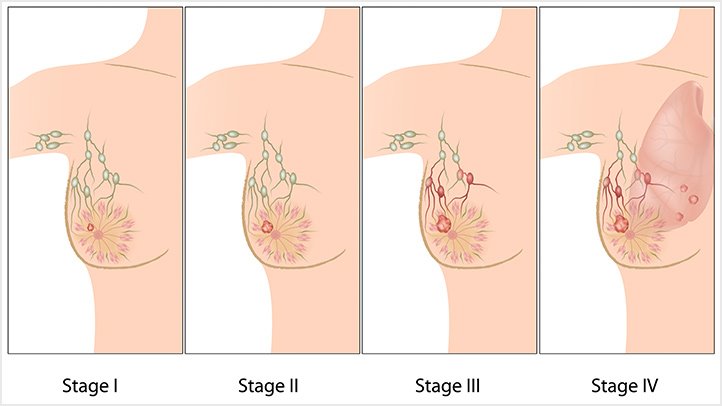
Different Stages Of Breast cancer
Breast cancer starts when cells in the breast begin to grow out of control. These cells usually form a tumor that can often be seen on an x-ray or felt as a lump. The tumor is malignant (cancer) if the cells can grow into (invade) surrounding tissues or spread (metastasize) to distant areas of the body. Breast cancer occurs almost entirely in women, but men can get breast cancer, too.Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about cancer and how all cancers start and spread, see Cancer Basics.
The stage of a cancer describes the size of the cancer and how far it has spread. Your breast cancer may be described as stage 1, stage 2, stage 3 or stage 4. The stage takes into account:
1.What are breast cancer stages?
- the size of the cancer
- whether the lymph nodes are affected
- if the cancer has spread to other parts of the body
Your specialist team will look at the stage, size and grade of the cancer, as well as the type of breast cancer, to help decide the most appropriate treatment for you.The difference between stage and grade can be confusing. If you’re not sure which one your specialist is talking about, ask them or your breast care nurse to explain it to you. You can also call our Helpline on 0808 800 6000 or use our Ask Our Nurse email service.
2. Stage 1 breast cancer
Stage 1 breast cancer is divided into two groups:
- stage 1A
- stage 1B
Stage 1A means the cancer is 2cm or smaller and hasn’t spread outside the breast.Stage 1B can mean:No cancer is seen in the breast, but a few cancer cells are found in the lymph nodes under the arm (known as micrometastasis)The cancer in the breast is 2cm or smaller and a few cancer cells are found in the lymph nodes under the arm (micrometastasis).
3. Stage 2 breast cancer
Stage 2 breast cancer is divided into two groups:
- stage 2A
- stage 2B
Stage 2A can mean:
No cancer is seen in the breast but cancer is found in one to three lymph nodes under the arm or near the breastbone .The cancer in the breast is 2cm or smaller and cancer is found in one to three lymph nodes under the arm or near the breastbone.The cancer in the breast is larger than 2cm but smaller than 5cm and no cancer is found in the lymph nodes under the arm.
Stage 2B can mean:
The cancer in the breast is larger than 2cm but smaller than 5cm. Cancer is found in one to three lymph nodes under the arm or near the breastboneThe cancer in the breast is larger than 5cm and no cancer is found in the lymph nodes under the arm.
4. Stage 3 breast cancer
Stage 3 breast cancer is divided into three groups:
- stage 3A
- stage 3B
- stage 3C
Stage 3A can mean:
No cancer is seen in the breast, but cancer is found in four to nine lymph nodes under the arm or near the breastbone.The cancer in the breast measures up to 5cm and cancer is found in four to nine lymph nodes under the arm or near the breastboneThe cancer in the breast is larger than 5cm, and cancer is found in up to three lymph nodes under the arm or near the breastbone.
Stage 3B means the cancer in the breast can be any size and has spread to the skin of the breast or chest wall. Cancer is found in up to nine lymph nodes under the arm or near the breast bone.
Stage 3C means the cancer in the breast can be any size, may have spread to the skin of the breast or chest wall and cancer is found in 10 or more lymph nodes under the arm or near the breastbone, or to nodes above or below the collarbone.
5. Stage 4 breast cancer
Stage 4 breast cancer cancer, also known as secondary breast cancer, can be any size, the lymph nodes may or may not contain cancer, but the cancer has spread (metastasised) to other parts of the body, such as distant lymph nodes, lungs, bones, liver or brain.If your cancer is found in the lymph nodes under the arm but nowhere else in the body you do not have stage 4 breast cancer.
6. TNM cancer staging system
Some doctors use the TNM staging system. This is a scoring system used to describe:
- the size of the cancer (T stands for tumour)
- the number of lymph nodes affected (N stands for nodes)
- whether there’s any spread of the cancer to other parts of the body (M stands for metastases)
Source: http://cancer.bloomarticles.com